How Can You Treat Patients More Quickly?
Fast simulation-to-treatment time in Radiation Oncology clinics is crucial. Find out how cancer care teams plan treatments more quickly with imaging software.
April 17, 2024
3 Ways Radiation Oncology Clinics Are Reducing Simulation-to-Treatment Time
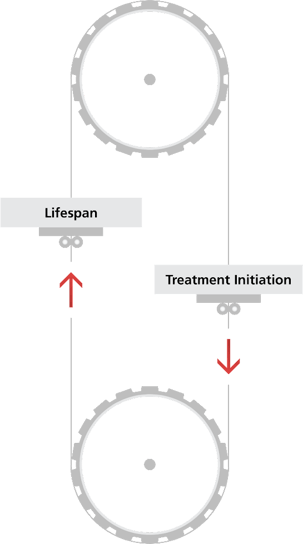
The sooner patients are treated, the better their outcomes. This was demonstrated in a recent study that evaluated more than two million cancer patients at 1,500 institutions over 11 years. The study found that for all types and stages of cancer evaluated, shorter time to treatment initiation (TTI) was associated with lower mortality.
This and other studies show the importance of treating patients quickly. Nonetheless, it’s getting more and more difficult for clinics to initiate cancer treatment promptly after simulation.
Various factors can make it challenging to treat patients quickly:
- Staffing shortages
- Increasing patient volumes
- Increasing frequency of cancer recurrence
- Growing complexity of treatment options
Despite Challenges, Clinics Are Shortening Patient Wait Times
Clinics are reducing TTI without compromising plan quality—even in an increasingly complex cancer care landscape.
Here are a few ways I’ve seen clinics of all sizes achieve faster simulation-to-treatment times:
1. Automate manual tasks at the point of simulation.
Manual processes are error-prone and can create bottlenecks that delay patient treatment. This is especially true for organs-at-risk (OAR) contouring. Clinics avoid bottlenecks by automating repetitive, time-consuming manual contouring work that unnecessarily burdens clinicians and takes away time for patient care.
Auto-contouring for OARs helps clinics shorten the path from simulation to treatment and take pressure off staff to maintain contouring results while keeping up with high patient volumes. At one clinic my team works with, full contouring automation has saved 45 minutes per patient.
2. Standardize best practices across the organization.
It’s difficult for care teams to initiate treatment quickly when their processes are inefficient and inconsistent. Inefficiency and inconsistency escalate when clinics onboard new care team members with varying experience levels.
Standardization helps clinics close the experience gap and keep the planning process moving without slowdowns. One of the easiest ways clinics can standardize processes is by implementing configurable workflow scripts that guide clinicians through common plan preparation tasks. These scripts make it easy for dosimetrists and physicists of all skill levels to prepare the information that physicians need to create target volumes.
This case study shows the role standardized workflow scripts play in simplifying staff onboarding and ensuring treatment quality across a large health system.
3. Give physicians tools to create target volumes more quickly.
Care teams need input from physicians as quickly as possible to unlock the next steps in the planning process and bring patients in for treatment sooner. Some common TPS limitations that increase physician contouring time include the inaccessibility of useful imaging data, unwieldy display configurations, and the need to estimate tumor location and size in complicated cases.
In my experience, clinics find the most success in reducing turnaround time for target-volume contouring when they:
- Systematically give physicians all needed information in one centralized place.
- Use QA tools that help them confidently assess the quality of registrations, regardless of complexity.
- Take advantage of automated contouring tools that set up physicians for consistent, repeatable accuracy.
For all the above actions, the results are the same: Inefficiency is minimized, physicians can start their work sooner, and most importantly: patients get treated more quickly.


